By Kurt T. Steele, OD
Dec. 15, 2021
Meibomian Gland Disease (MGD) is found in most patients with dry eye disease (DED). Here is a new approach to addressing MGD that can greatly help both patient outcomes and practice profitability.
Are You Addressing the Real Problem?
For the longest time, eyecare providers tried to solve our most frequently encountered ocular pathology by treating the symptom, not the problem. The problem with dry eye disease appeared simple with the belief that patients did not make enough of their own natural tears. The solution also seemed simple…replace natural tears with artificial tears to replenish the system. Based on this clinical insight, the industry provided various treatments from OTC artificial tears to advanced pharmaceutical options for patients to make more of their own tears. Unfortunately, none of these options addressed the true underlying problem staring at us in clinic.
In many cases of dry eye, the patient’s lacrimal gland is functioning properly and producing enough tears for a normal, healthy experience without symptoms of dry eye. Producing tears is not the issue; helping patients retain their own natural tears before they evaporate is our challenge. The outermost oily layer of the tear film functions to prevent evaporation of the aqueous portion of the tears. When meibomian glands become blocked or atrophy altogether, the loss of protective oils accelerates the evaporation of patients’ natural tear film.
In 2012, Lemp published a hallmark study noting that 86 percent of patients in clinic should now be classified as having MGD or Evaporative Dry Eye.1 MGD is a chronic condition caused by an obstruction in the meibomian glands (MG), which if left untreated, can lead to eventual gland atrophy and dropout.
TFOS DEWS II details the current standard of care for a DED and MGD treatment algorithm as a starting point for all our patients.2 It is simple, and yet not routinely followed by many clinicians. By educating each patient on what causes their MGD and the role their oily layer plays in maintaining a healthy ocular surface, the importance of taking care of their lids starts to become apparent to our patients.
In my clinical experience, one of the most important items in this treatment algorithm is daily heat therapy, which is critical if we are to effectively address the underlying issue of MGD obstruction. As clinicians, we have always known patients require daily heat therapy and lid hygiene. But current heat and lid hygiene regimens are too complicated, and most patients quickly give up on this critical therapy. As stated succinctly by Marguerite McDonald, MD, regarding dry eye, “Non-compliance is the #1 problem with our #1 problem in practice today.”
Dry Eye patients are our most frustrated patients. They have bounced around from clinician to clinician, always being given the same treatment options. Different brands of tears, clunky and inconvenient heat therapy, and/or lid hygiene in varying forms. Similarly, many ECPs have also grown frustrated and given up on certain heat therapy or lid hygiene treatments because of the overall non-compliance. Our patients will always follow the path of least resistance.
If our treatment does not fit into their lifestyle, then we are pushing water uphill. Historically, we recommended that all our patients use some form of hot soaks, scrubs or microwaveable masks. Unfortunately, most patients simply give up due to ineffectiveness or the inconvenience of having to use multiple products or break from their normal routines to use a microwave (which is often not particularly sanitary). We need easier, better options and more convenient solutions for our patients if we are going to truly advance patient care for these MGD and dry eye patients.
Precise Science & Technology
Most recently, I had the opportunity to be an Early User site for a new heat therapy technology developed by Professor Michel Guillon of the Ocular Technology Group in London. Dr. Guillon’s new MGD therapy incorporates two “standard of care” technologies into one product by bringing precise heat therapy and lid hygiene into a simple, easy-to-use and affordable product called “EverTears®.”
The product was featured in the 25th Edition of “Clinical Perspectives On Patient Care” by Drs. Ron Melton, Randall Thomas and Patrick Vollmer, which highlighted EverTears® as the world’s first self-heating compress + pre-moistened cleaning pad that provides an easy, convenient and affordable technology for our MGD patients.
EverTears® technology provides instant heat quickly. Within seconds, the individually wrapped pads are ready to use and at the precise temperatures to ensure 90 percent liquification of the meibum. EverTears® precise heat will maintain temperatures > 40° Celsius for around six minutes and over 38° Celsius for eight minutes. This allows adequate time for patients to use one pad to treat both eyes. Additionally, EverTears® uses a proprietary cleaning formulation that includes Sodium Hyaluronate, PEG and coconut extracts to ensure the lids stay free of debris.
My patients found it convenient to use EverTears® for two minutes per eye and easy to incorporate this therapy into their busy lifestyle. I tell patients to put the individually wrapped EverTears® on a nightstand, use it in the shower or wherever it is most convenient so that they remember to use it every day. The fact that each pre-moistened pad is individually wrapped also makes it easy for patients to use EverTears® while traveling, at work or the gym or simply as part of their daily routines like makeup removal at the end of the day.
The best part is that there are no more non-compliance excuses. We now have an OTC product that is convenient. Unlike artificial tears, EverTears brings a treatment solution to the root cause of most dry eye cases…MGD. In my 26 years in practice, this is the single biggest breakthrough I have seen in the dry eye space that all clinicians can access for their patients.
Based on the findings of Lemp and others, we now know that the progressive nature of this disease and gland atrophy can be managed if we do a better job of staying focused on the underlying problem, which is treating the MG obstruction. If keeping the meibomian glands healthy and functioning properly remains our primary objective, then perhaps we must first update our treatment algorithms.
Strong OSDI Results
As with many new products, I always bring a healthy dose of skepticism, but I was excited about the potential for a product that might be able to deliver the solution they claimed. First, I tried it on myself and noticed a difference on my own symptoms of dry eye, both in comfort and helping with my end-of-day intermittent blurring.
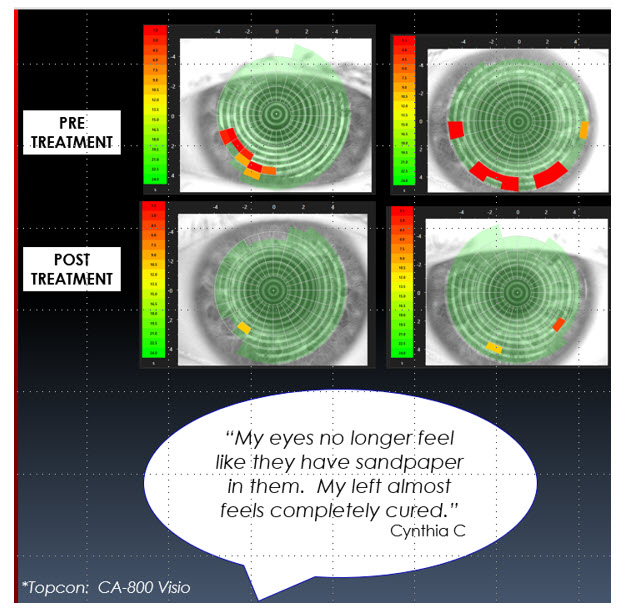
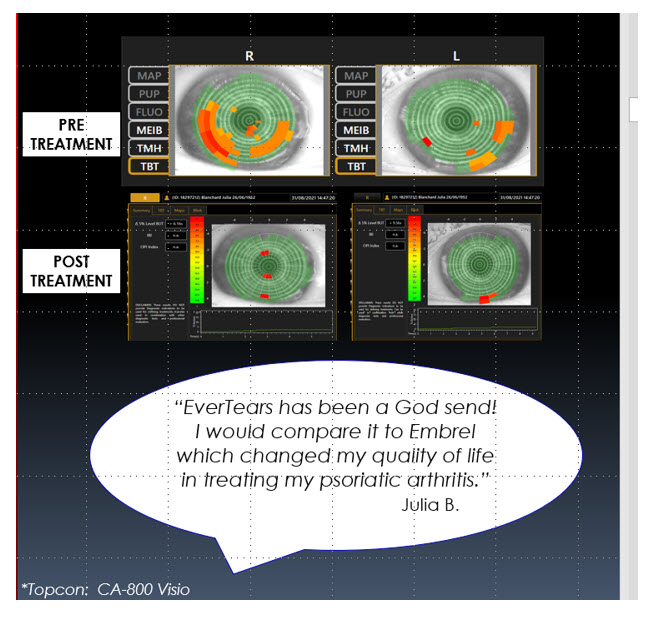
As a practice of three ODs, we decided to try it on dry eye patients and use the OSDI instrument and Topcon meibography to determine if the product delivered improvement in symptoms and signs. We used one pad with each patient in the chair to show how easy it is to use every day and how good it feels on the eye. Then we recommended EverTears® B.I.D. for one week followed by Q.D. until their return visit to the office. After three weeks using the product, the results exceeded my expectations.
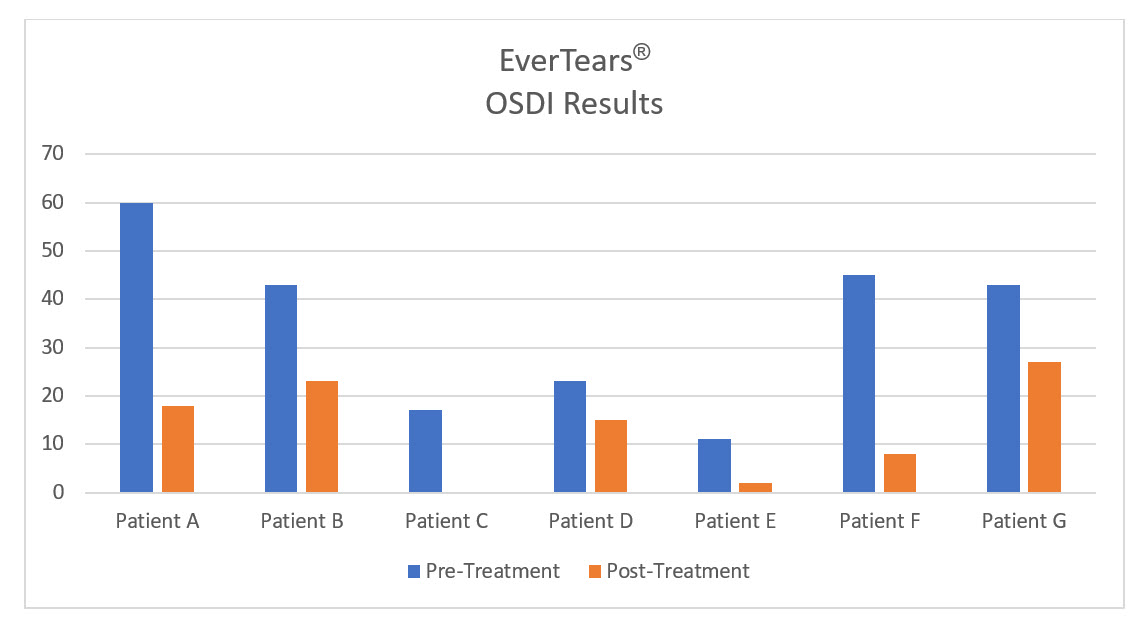
Overall, the OSDI results and patient feedback regarding EverTears® were outstanding. Two of seven patients improved two full grade levels, and the remaining five patients improved one level or showed significant improvement from baseline. Although Patient E was technically asymptomatic because the OSDI instrument does not contain a question about watery eyes (the primary complaint of Patient E), his clinical results demonstrated improvement and he was one of the happiest, most enthusiastic patients about the treatment’s benefits.
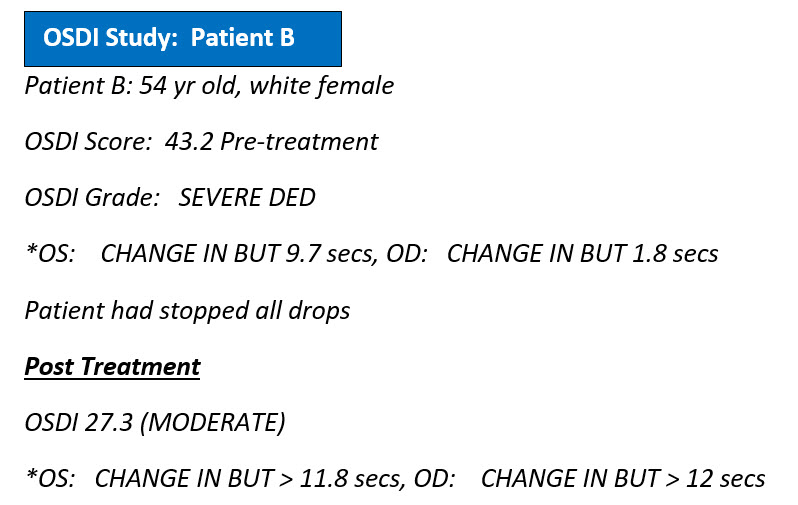
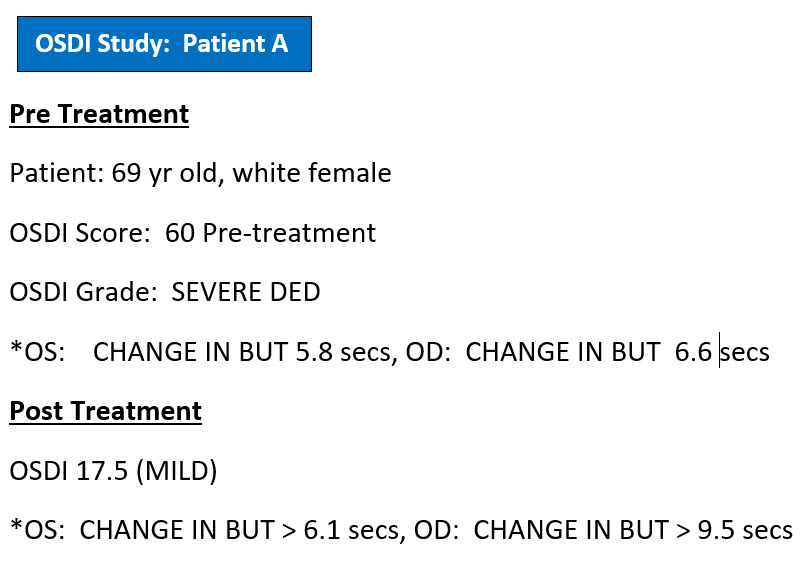
Additionally, shown below are a few of the improvements made in the objective clinical measures for two of the severe patients and their comments on how they felt after three weeks of treatment. Both patients felt significant improvement from their baseline measurements. Each patient was classified as according to the pre-treatment OSDI measures. One patient improved two grades to mild and the other improved one grade to moderate in the post-treatment evaluation after using EverTears three weeks.
Since we have begun using EverTears® in the practice, we have treated well over 100+ patients with the technology. Around 90 percent of the DED/MGD patients purchased EverTears® after their initial follow-up visit at one month post-treatment.
Summary
Like many practitioners, it is easy to become enamored with the latest trends that have been hailed as breakthroughs for dry eye, MGD or ocular surface disease. Yet despite all our advancements, patients are still frustrated because we still have not consistently resolved their main underlying problem, which is the MG obstruction. We continue to complicate the treatment regimens required for these patients. It is easy to simply hand patients a sample of artificial tears, but then we lose focus on the real problem, and it’s our patients who will continue to suffer.
If you use artificial tears before any other treatment for symptoms of dry eye, I ask you to pause and reset your own treatment algorithm. As clinicians, we need to work hard at addressing the underlying gland obstruction and get back to the fundamentals of what is required to effectively manage the majority (as high as 86 percent) of our patients who have MGD.
Let’s put our focus on the lids and daily lid care/hygiene and get the patient’s own natural tears and system working better, rather than defaulting solely to symptom relief with treatments like artificial tears.
References
1. Michael A Lemp et al. Cornea. 2012 May, Distribution of aqueous -deficient and evaporative dry eye in a clinic-based patient cohort: a retrospective study
2. The Ocular Surface. 2017 July, TFOS DEWS II Report Executive Summary
 Kurt T. Steele, OD, is a Partner of Vision Source of Newport in Newport, Tenn. To contact him: idoc2316@gmail.com
Kurt T. Steele, OD, is a Partner of Vision Source of Newport in Newport, Tenn. To contact him: idoc2316@gmail.com


























