By James E. Grue, OD,
Ronald P. Snyder, OD, FAAO,
Michael J. Lipson, OD, FAAO, FSLS,
and Greg Caldwell, OD, FAAO
July 14, 2021
Asking your patients about their health concerns provides essential information that is necessary for you to transition your practice to provide patient-centered care. Here is how to do that, and why doing so will benefit both your patients and practice.
What is Patient-Centered Care?
Patient-centered care is defined as providing care that is respectful of, and responsive to, individual patient preferences, needs and values, and ensuring that patient values guide all clinical decisions. This approach requires a true partnership between individuals and their healthcare team.
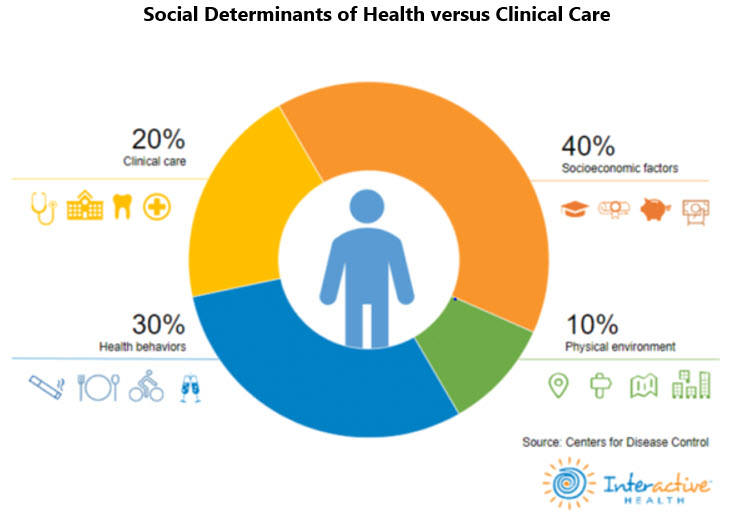
Figure 1
Demonstrates Social Determinants of Health (80 percent) versus Clinical Care (20 percent). This image was taken from a recent presentation made by The Office of the National Coordinator of Health Information Technology (ONC).
As seen in the figure above, 80 percent of a person’s health and healthcare is determined by social factors such as socioeconomic factors, health behaviors and physical environment.
When we make recommendations to our patients based on clinical care without considering social factors, data suggests we fall short of realizing ideal outcomes. Practitioners often do not recognize the influence of the social factors, but it is impossible for the patient to ignore these concerns. These social factors, commonly referred to as Social Determinants of Health (SDOH), are often the cause of poor clinical outcomes. A patient can receive excellent medical care, but if they can’t afford their medications, or don’t have access to proper food and hygiene, clinical outcomes will be adversely affected.
What Can I Do About “Social Factors?”
Historically, medicine has largely ignored SDOH in recommending care. As a provider, you may feel “I can’t do anything about these social factors,” but that is not true. Let’s look at two specific situations.
1. A patient requires five different medications, but doesn’t have the financial resources to purchase all of them.
If the care team isn’t aware of the patient’s financial hardship, and doesn’t assist the patient in addressing this concern, the patient may forego purchasing some or most their medications. If the care team had considered this situation, they may have been able to prescribe a substitute or generic, so the patient could afford to purchase all five medications. Most certainly, it would be better for the care team to address this situation than to leave the patient to deal with it alone.
2. Another consideration of SDOH is understanding what a patient “thinks” about their care.
In this example, let’s look at what a patient “thinks” when they find out that they are diabetic: “Every one of my family members with diabetes has lost vision. It is inevitable that will happen to me, too.” When a patient thinks about their care with a biased perspective, it is easy to see how this can lead them to make poor decisions in how they manage their condition. The patient may have physical limitations that become an obstacle to medical care. A pharmacy or supermarket may not be conveniently located either.

To learn more: 844.393.3282. (toll free) or ContactUs@HealthCareRegistries.com
The point is, if you are not considering the SDOH that may be affecting your patient’s overall health, you may be missing important information that would allow you to deliver more targeted care that works better for each unique situation.
To find out the health concerns of your patient, ask these two sample questions:
1) “When you think about your diabetes, what worries you? What concerns about your diabetes keep you awake at night? “
2) “What challenges are keeping you from getting better control of your diabetes? What makes it difficult for you to improve your control? “
Your skill in asking these questions will get your patients thinking and sharing their health concerns with you. This will result in you becoming aware of a whole new world of information and having a newfound understanding of your patients.
When you begin asking these questions, the results are predictable:
• Your plan of care will never look like it did in the past.
• The communications and discussions you have with other members of the patient’s healthcare team will significantly change. Your care plan will have a direct and measurable improvement in clinical outcomes.
• This new approach will show you clear ways to improve referral relationships with other members of the care team. It also positions your practice as the one primary care physicians (PCPs) refer their patients to for eyecare.
• You will have a much better understanding of how your practice fits into the emerging patient-centered, coordinated, outcome-based care delivery system that healthcare reform is driving in the country.
• As a profession, the resulting clinical outcomes data will help establish the basis for payers to develop alternate payment systems that reward providers who demonstrate improved outcomes for eyecare, as they do for PCPs.
Other Articles to Explore
Action Plan
We challenge you to do two things:
1) Commit to asking those two questions of your next 10 “uncontrolled” diabetic patients. When you do, you will see the power of the information patients can provide you, and you will never stop asking those questions.
2) Share with us some of your interesting patient responses. In our next article, we will address these patient responses and explain how to handle the various scenarios.
This approach to patient-centered care is new to most eyecare providers. We are just beginning to appreciate the power of this approach. We are going to make the most rapid progress as a profession if we use a collaborative approach in which we share among providers how these issues are addressed and together watch the impact on clinical outcome measurements. Your practice can be part of this collaborative process.
 James E. Grue, OD, is a health-care reform speaker and consultant. To contact him: JimGrue@HealthCareRegistries.com
James E. Grue, OD, is a health-care reform speaker and consultant. To contact him: JimGrue@HealthCareRegistries.com
 Ronald P. Snyder, OD, FAAO, is the president and CEO of HealthCare Registries, LLC. To contact him: RonSnyder@HealthCareRegistries.com
Ronald P. Snyder, OD, FAAO, is the president and CEO of HealthCare Registries, LLC. To contact him: RonSnyder@HealthCareRegistries.com
 Michael J. Lipson, OD, FAAO, is the chairman of the OrthoK Advisory Panel of HealthCare Registries, LLC.
Michael J. Lipson, OD, FAAO, is the chairman of the OrthoK Advisory Panel of HealthCare Registries, LLC.
 Greg Caldwell, OD, FAAO, is Chairman of the Advisory Panel for the Diabetes Management Registry.
Greg Caldwell, OD, FAAO, is Chairman of the Advisory Panel for the Diabetes Management Registry.