By Mark K. Davis, OD

July 19, 2023
Optometry and ophthalmology are fortunate in that the professions generally have two ways to describe and bill for a medical office visit. An in-depth discussion of each set of codes is beyond the scope of this article.
I will attempt to give an overview. Also, you may find that some optometrists prefer E/M codes, some prefer only ophthalmology codes and some, such as myself, use both. There is no wrong answer.
Let’s take a look at each set of codes.
Evaluation & Management codes are defined as the following:
History and Examination – as medically appropriate, NOT used in code selection. (this was a big change in 2021, we get to be doctors!)
Time – Face-to-face time with the patient and/or family, which includes time spent obtaining history, examination, counseling the patient, ordering medications, tests or procedures, referring and communicating with other healthcare professionals, documenting clinical information in the EHR or other health record, independently interpreting results (not separately reported) and communicating results to patient/family/caregiver, care coordination (not separately reported). This does NOT include your staff time with the patient.
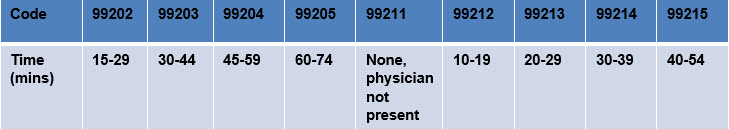
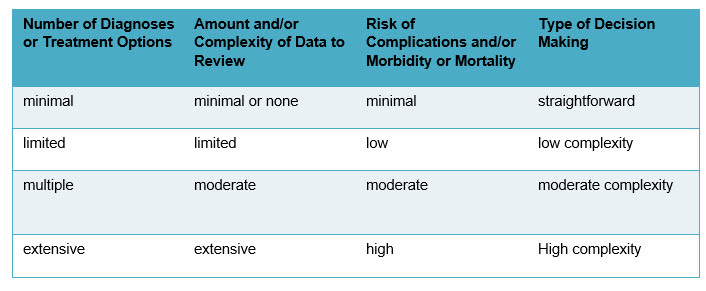
Medical Decision Making (MDM) – use key components (history, examination and MDM)
Elements of MDM lead to the following chart of the Complexity of Medical Decision Making: (for an in-depth explanation, see Guidelines for Office or Other Outpatient E/M Services in the CPT codebook)
I did a small survey of my physician friends that are in the USAF Reserves with me and also practice in the civilian world versus my civilian optometry friends. Survey says, most physicians use the MDM model for coding and most optometrists use the Time model for coding.
My physician friends tell me they can get paid more using the MDM model. They already have the office visits on charts they can refer to based on the most common patient disease diagnosis (think diabetes, hypertension, cholesterol, etc) and if they are under control or not. These charts are often provided by their professional groups. Other physician friends rely on what the EHR tells them to code. I am cautious about this, especially if audited. I would hate to say to the auditor, “Well that’s what the EHR said to use.” You have to be knowledgeable enough to back up your choices, and the provider is ultimately responsible for any errors.
Optometry, on the other hand, uses time more frequently because we usually have “time slots” (15 minutes, 20 minutes, etc.) on our schedules. We generally want to see X number of patients in an hour.
Other Articles to Explore
Now let’s look at the ophthalmology codes. They are defined as the following:
Intermediate ophthalmological – describes an evaluation of a new or existing condition complicated with a new diagnostic or management problem not necessarily relating to the primary diagnosis, including history, general medical observation, external ocular and adnexal examination and other diagnostic procedures as indicated; may include the use of mydriasis for ophthalmoscopy.
Comprehensive ophthalmological – describes a general evaluation of the complete visual system. The comprehensive services constitute a single service entity, but need not be performed at one session. The service includes history, general medical observation, external and ophthalmoscopic examinations, gross visual fields and basic sensorimotor examination. It often includes, as indicated: biomicroscopy, examination with cycloplegia or mydriasis and tonometry. It always includes initiation of diagnostic and treatment programs.
What is so nice about the ophthalmology codes is that they are based on examination only! Optometrists are great at doing comprehensive eye exams and office visits. You don’t have to worry about time or MDM, just what you find on examination.
I have many friends that use only ophthalmology codes. If you are one of these individuals, when billing Medicare, pay particular attention to the following statement. I have heard from numerous sources that frequencies in excess of the unwritten, but standard, industry average of 60 percent comprehensive and 40 percent intermediate, will often times trigger an audit. You cannot do a comprehensive exam on all patients. You have to go by the patient’s chief complaint, as to what type of examination you perform.
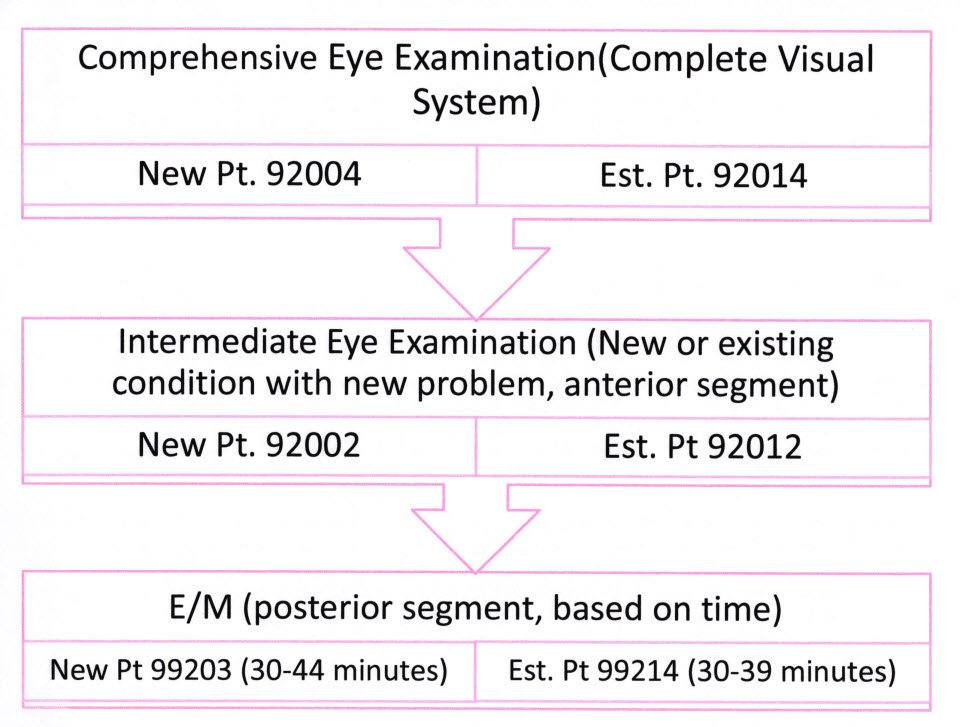
So, what did I use when I had my private practice?
I felt that 92002 or 92012 was more for the anterior segment based on the part of the definition stating “general medical observation, external ocular and adnexal examination and other diagnostic procedures as indicated.” Also, I felt if I was going to spend a fair amount of time looking at the posterior pole for, say a possible retinal detachment, I wanted to get paid more than what the 92002 or 92012 paid. So, for the posterior pole, I generally used the E/M codes and based it on time. Remember, I’m a simple person (yes, there’s a joke in there).
I generally went by the following chart.
Most of this information I have provided can be found in the CPT Code Book published by the American Medical Association annually. I myself scour it for any changes, additions or deletions every year.
 Mark K. Davis, OD, is a Therapeutic Optometrist and Optometric Glaucoma Specialist, Diplomate, American Board of Optometry, Adjunct Assistant Professor, University of Houston College of Optometry and Chief of Optometry, 147th Medical Group. He is Lt Col, Texas Air National Guard, Ellington Field JRB, Houston, Texas.
Mark K. Davis, OD, is a Therapeutic Optometrist and Optometric Glaucoma Specialist, Diplomate, American Board of Optometry, Adjunct Assistant Professor, University of Houston College of Optometry and Chief of Optometry, 147th Medical Group. He is Lt Col, Texas Air National Guard, Ellington Field JRB, Houston, Texas.

























