By Peter J. Cass, OD

April 22, 2020
The COVID-19 crisis has significantly challenged all of our practices. One improvement that may come from surviving the pandemic is greater use of telehealth to provide ongoing care and satisfy patients’ desire for telehealth visits with their doctor.
CMS has recognized this need and relaxed the rules for telehealth making it easier than ever for providers to offer these services to patients. Use of this technology, however, won’t benefit your practice if you can’t get paid for it. Here are tips on coding for telehealth patient appointments.
First you need to understand the different types of telehealth services available. Currently there are four:
1. Virtual Check Ins
2. Telephone Services
3. On-Line Digital Evaluation
4. Telehealth Services
Normally co-pays and deductibles apply to these services, but CMS has indicated that they can be waived during the COVID-19 crisis. These services typically cannot be provided when you have seen the patient within seven days before the service, or the service results in an office visit within 24 hours. Also note that they cannot be billed to monitor post-op status (as this is already included in global fee). Private payors may or may not cover these services.
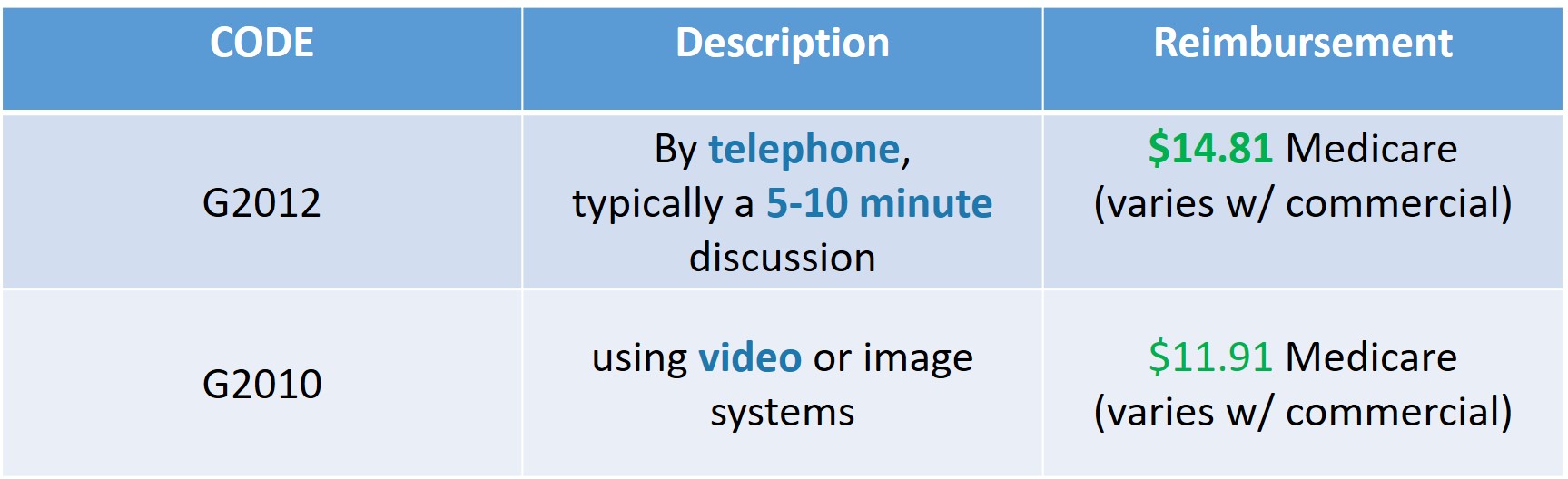
1. Virtual Check In
This service is used to “check-up” on a patient where you are monitoring their status, symptoms or their response to treatment. When providing these services:
• Confirm patient identity (e.g., name, date of birth or other identifying information as needed)
• Document the total amount of time spent (only submit code G2012 if a minimum of five minutes of direct communication with the patient was achieved)
• Confirm that the patient provided consent for the service.
The service is billed using the following codes:
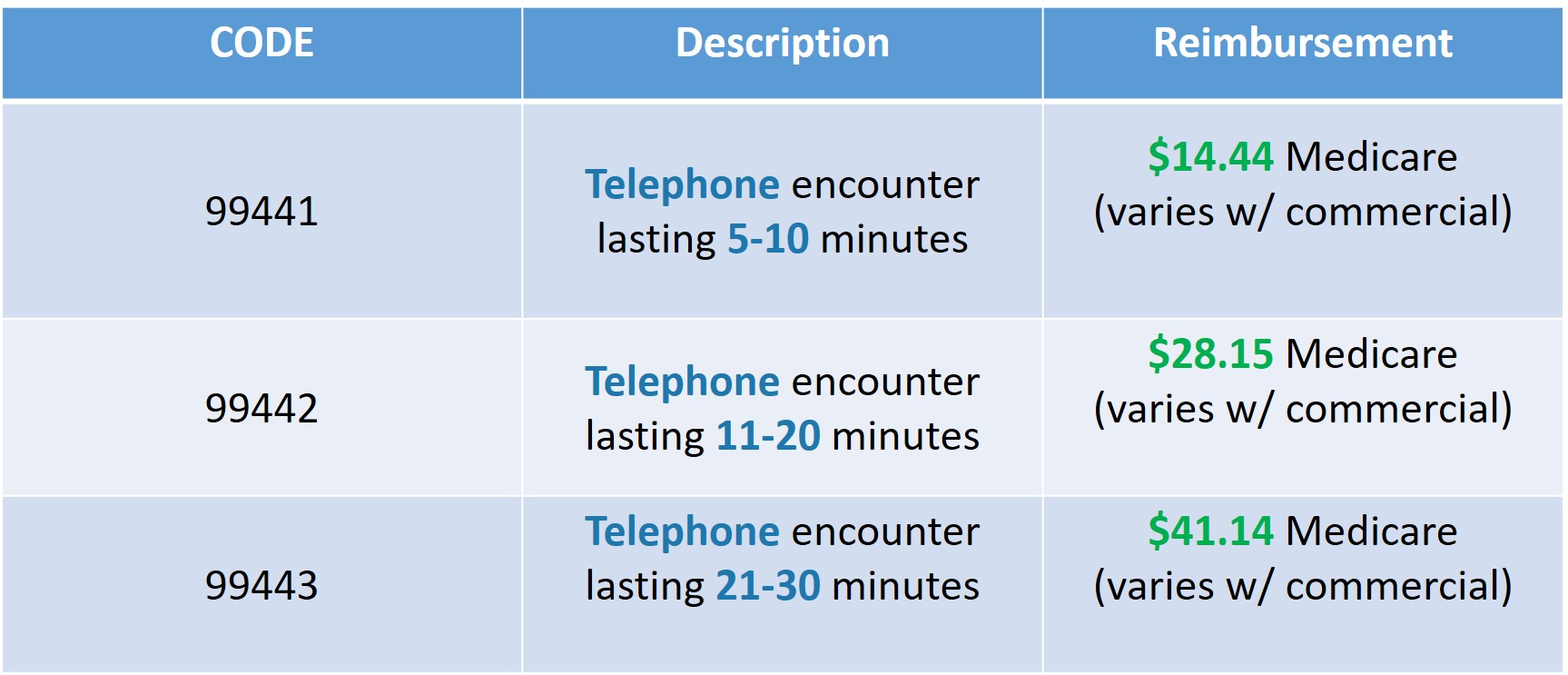
2. Telephone Services
These are telephone consultations that are initiated by the attending physician to follow-up on a patient’s status. In the past CMS has not recognize this service, but is allowing it during the COVID-19 crisis. When providing these services, you should document:
• Patient’s verbal consent for services
• Pertinent history
• Patient’s present medication use
• Treatment recommendations
• Total time of medical discussion
The service is billed using the following codes:
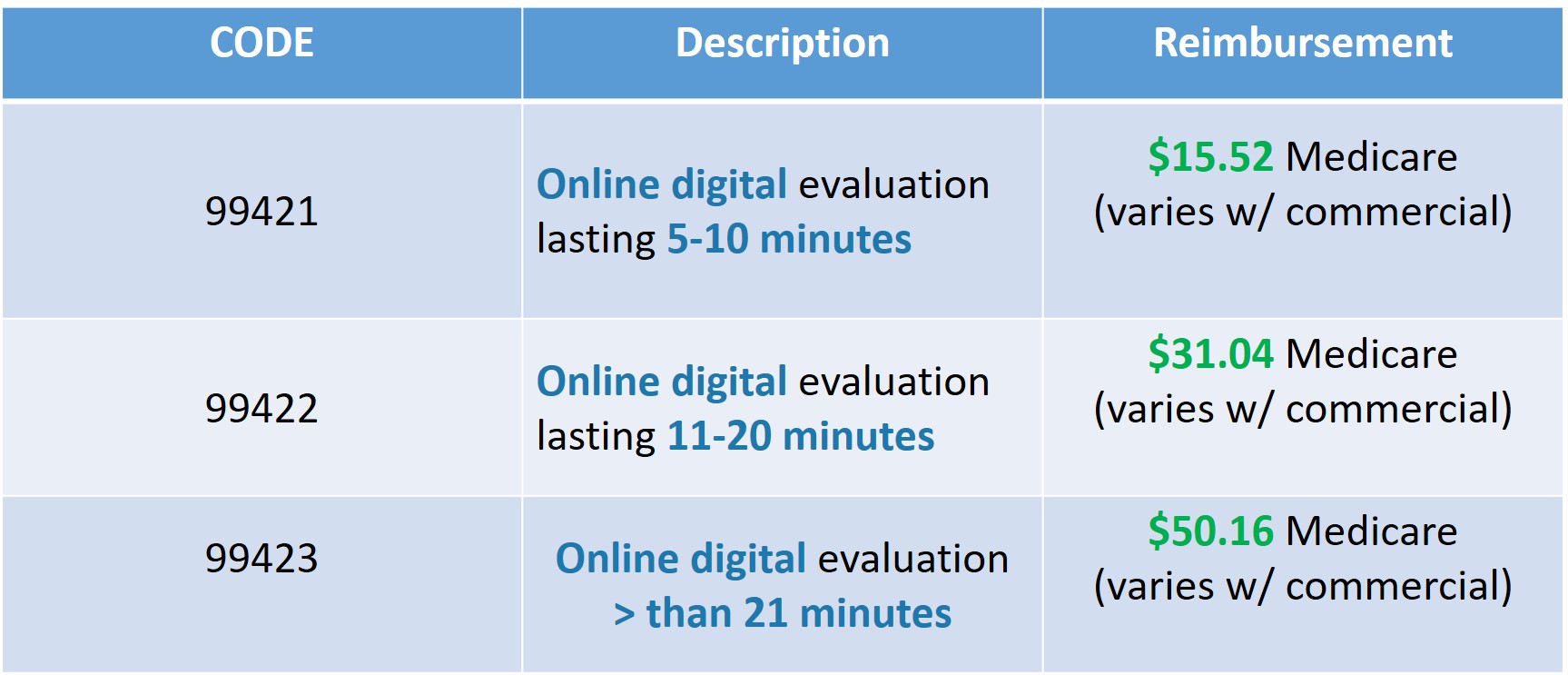
3. Online Digital Evaluation
This is a teleservice that occurs mainly using the practice’s electronic medical record portal. It would also involve the use of video or image review and communication with the patient. When providing these services, all aspects of the encounter should be documented in the patient’s electronic medical record
The service is billed using the following codes:
4. Telehealth Services
This is a remote patient evaluation using real time, interactive, two-way audio/visual communication systems. In the past these services were restricted to counties outside the Metropolitan Statistical Area (MSA) or inside a Health Professional Shortage Area (HPSA) and could not be proved to patients in their home, however CMS has relaxed these requirements during the COVID-19 crisis.
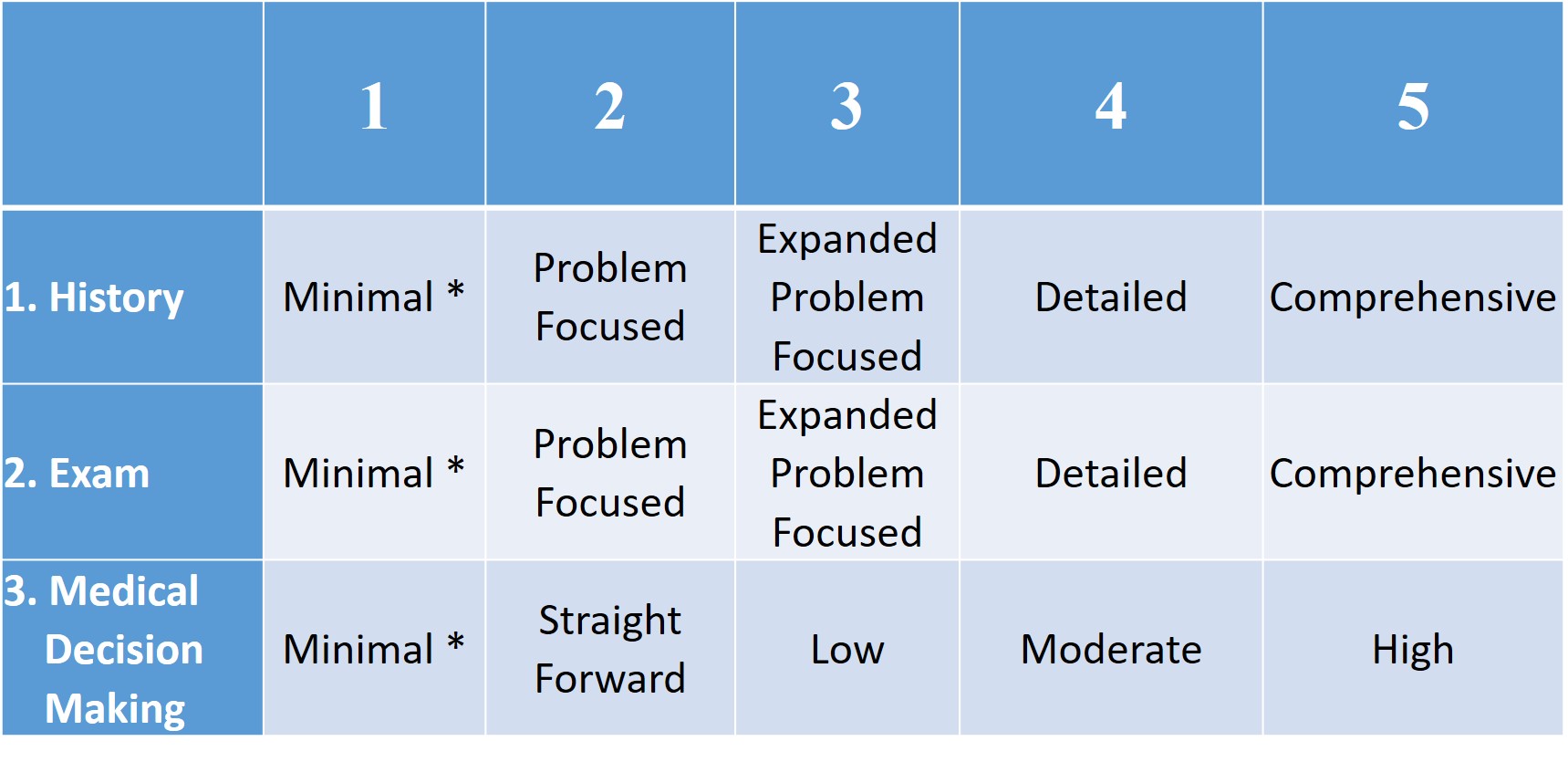
The service is billed using the following codes:
Other Articles to Explore
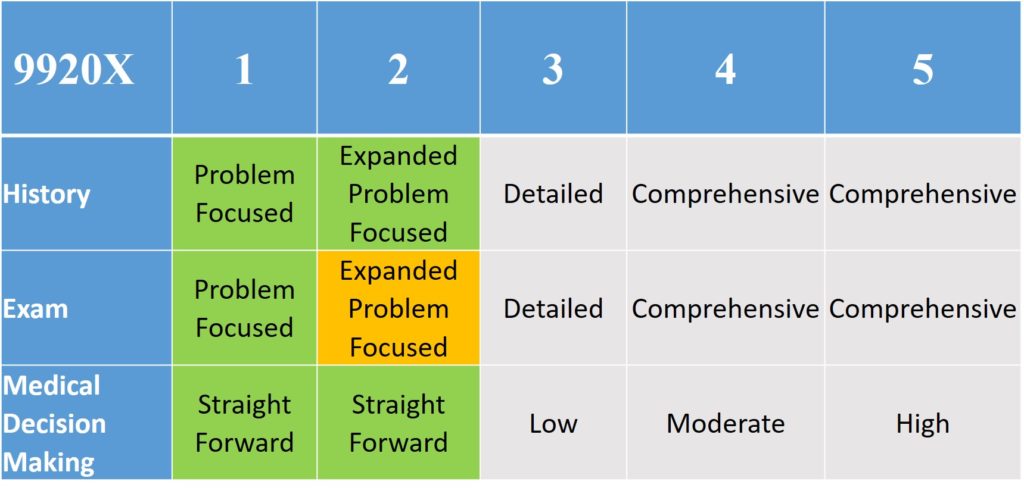
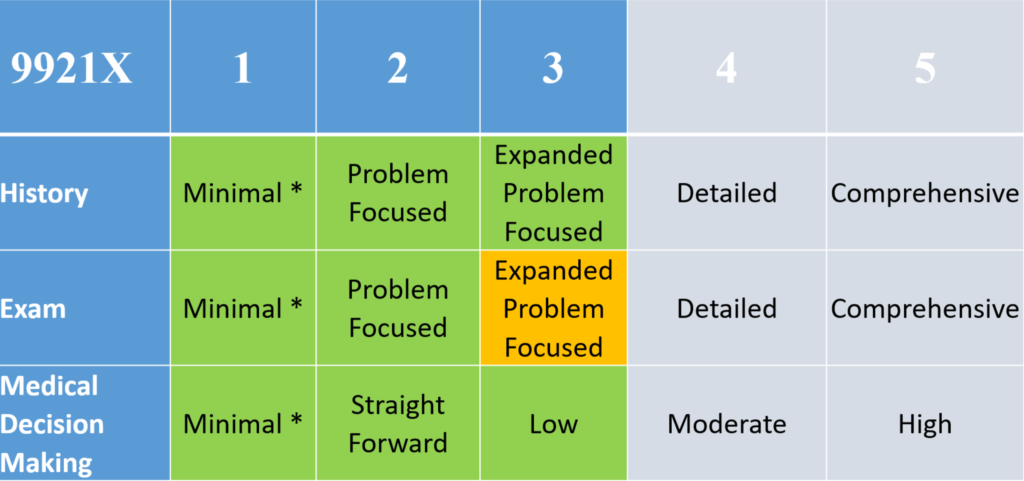
The regular evaluation and management codes (9920X, 9921X).
It is not payable for ophthalmologic codes.
Use of the -95 modifier is recommended
The place of service code for these services is – 11 (normally 02-telehealth)
While the criteria for selecting the code level are exactly the same as for in-office services, there is certainly a limit on the number of examination elements that can be conducted using remote technology, which can be a limiting factor in code level determination. It would be difficult to achieve higher than a level 3 established or a level 2 based on exam elements required for those codes. Time can be used as the single determining factor or code level selection can be used, and if used, should be documented properly.
Additionally, for all telehealth services, HIPAA privacy rules were relaxed and CMS has stated that no investigations or audit of services will be conducted – but only related to these telehealth services. HIPAA did not go away. CMS is allowing non-HIPAA compliant platforms for use in telehealth during the COVID crisis as long as they are not public facing. Examples given include: Apple FaceTime, Facebook Messenger video chat, Google Hangouts video, Whatsapp video chat and Skype.
Telehealth and Other Payers
CMS actions are not binding on other health-care payers. Each payer is likely to make its own rulings regarding any action related to telehealth services during the COVID-19 crisis. Individual states also may have regulations regarding telehealth services that could affect optometric provision of these services outside of the CMS system. States are likely to also implement emergency rulings to increase access to telehealth services.

Peter J. Cass, OD, is the owner of Beaumont Family Eye Care, a Vision Source practice in Beaumont, Texas, and past-president of the Texas Optometric Association. To contact: pcassod@gmail.com

























