By Thomas F. Steiner
 Director of Market Research,
Director of Market Research,
Review of Optometric Business
May 20, 2015
Second in the series “Differentiating Your Practice”
SYNOPSIS
Fees are increasingly limited as managed care grows, but wisely managing your product mix can ensure practice profitability.
ACTION POINTS
PROVIDE THE RIGHT MIX. Include in your offerings premium vision correction options that bolster revenues by not being widely available elsewhere.
MAKE IT ABOUT PRODUCT BENEFITS. When patients understand the personal benefits of premium vision options, concerns about higher costs fade.
EQUIP YOUR STAFF TO EDUCATE. The message your staff projects to patients is key to succeeding with differentiated products.
Over the past 50 years, independent ECPs have seen a steady decline in the share of revenue from direct-paying patients and a corresponding increase in share of revenue from managed care payers. This highly significant change in daily practice is a trend evident in nearly every medical specialty.
The spread of employer-sponsored vision insurance plans and increased government funding are the key drivers of managed care growth in vision care. Currently, direct patient payments account for a steadily shrinking one-third of revenue ODs receive, and managed care for the remaining two-thirds. The ratio varies widely among practices. But today, very few ECPs can afford to refuse participation in managed care and retain total control over the fees they charge. All third-party provider ECPs must accept the terms imposed by managed care payers on what patients can be charged for goods and services.
“Specialty CLs Warrant a Higher Fitting Fee”
Brian D. Brightman, OD
Eyecare Specialties
Lincoln, Neb.
www.eyecarespecialties.com
Every day, Brian Brightman, OD, president of Eyecare Specialties in Lincoln, Neb., navigates the financial challenges posed by managed care—specifically, the profit margin pressures associated with decreasing reimbursements. His strategy for success is to specialize in fitting premium contact lenses.
For patients opting for new high-tech CL options, Dr. Brightman charges patients a higher fitting fee “commensurate with the technology and the special fitting process.” This fee is approximately 50 percent higher than the practice’s standard lens fitting fee.
“We essentially give patients two options: They can have a standard fitting, and get a lens they can buy anywhere, or they can undergo a more comprehensive fitting and receive the best lens available,” he explains. “That process requires extra time, and it makes sense to charge a higher fee for that service, particularly in the managed care era. Your time has value.”
At Eyecare Specialties, patients are asked to consider their insurance as a “voucher” toward this premium service. Dr. Brightman provides added value in return—essentially a fitting that is “almost like a pre-operative consultation.” All patients undergo corneal topography, and Dr. Brightman shows them a three-dimensional view of their corneas and describes how a specific lens design will work and how it will effectively conform to their unique needs. He has found particular success with scleral lenses and hybrid designs such as Duette from SynergEyes.
“These lenses have better optics than softer designs, basically the vision of a rigid lens but the fit of a softer lens,” he explains. “It’s a product that fits right in with our philosophy of offering the best technology, along with our topographer and our goal of getting eyeglass wearers into glare-free and digital [spectacle] lenses. We are constantly looking for ways to distinguish ourselves by offering the best products available.”
Health care reform to put a new squeeze on ECP reimbursement
It’s highly likely that health care reform will accelerate the market share increase of managed care in eyecare. Regardless of which political party retains control of Congress or the White House, it appears virtually certain that significant reforms in how healthcare is delivered in the US will unfold in the years ahead. That’s because the current system is unsustainable, with structural flaws that limit patient access, reduce efficiency and quality of care and raise costs at a faster rate than general inflation.
Likely developments stimulated by health care reform that will impact independent ECPs include:
• Increased patient access to care. The number of people enrolled in insurance plans will grow and managed care payers will gain additional leverage over providers. A positive result for most ECPs will be an increase in the number of patient visits.
• Consolidation within the insurance industry. Greater government regulation of health care will create national standards for care regimens, reimbursements and outcome reporting, all of which will favor larger insurance firms. It will become increasingly problematic for ECPs to avoid accepting plans of the dominant insurers. The large insurers will have strong leverage to dictate terms to their provider networks.
• Increased administrative burdens for providers. Government and insurance payers will impose new reporting requirements. EHR adoption will become mandatory.
• Stagnant or declining reimbursements. Government and insurance payers have few acceptable options to reduce healthcare costs. Rationing and restricted formularies are unpopular with consumers, who have choice among insurance plans. Device or treatment price controls would slow innovation. It is easiest for managed care payers to contain costs by limiting provider reimbursements. Providers dependent on managed care payments have little recourse to affect reimbursement levels.
These developments, particularly stagnant and declining reimbursements, pose a significant threat to the revenue model of many independent ECPs. That’s because chair costs in typical practices, which rise every year, usually exceed reimbursements of managed care payers.
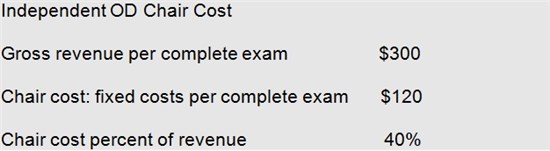
Data from the Management & Business Academy, sponsored by Essilor, show that for independent ODs, a typical patient visit generates about $300 in gross revenue. Of this amount, about $120 in expense is incurred for the fixed costs of keeping the office open for business (staff, rent, utilities, general overhead, equipment, etc.), collectively referred to as chair cost. If a practice fails to sell a vision correction device to a managed care patient at a profit, it’s unlikely that reimbursement for professional fees will offset chair cost. For this reason, retaining device sales in the practice is critical.
 There are no published industry norms for typical revenue derived from a managed care patient versus a direct-pay patient, but it is likely that the median revenue is $50 to $100 less. If managed care reimbursements do not keep pace with inflation over time, and fixed costs continue to grow at 2-3 percent annually, it’s clear that profitability will rapidly erode.
There are no published industry norms for typical revenue derived from a managed care patient versus a direct-pay patient, but it is likely that the median revenue is $50 to $100 less. If managed care reimbursements do not keep pace with inflation over time, and fixed costs continue to grow at 2-3 percent annually, it’s clear that profitability will rapidly erode.
Product mix management more critical under health care reform
ECPs have a limited number of strategies to preserve profitability in a world of shrinking reimbursements:
• Reduce fixed cost of providing service. Increasing office efficiency can reduce the amount of time spent with each patient and lower staffing cost per visit. This strategy has limits and runs the risk of lowering patient perceptions of service.
• Raise professional fees to direct-pay patients. This is an effective strategy, but also has limits. As the share of revenue generated by direct-pay patients shrinks, this strategy will yield less and less.
• Raise prices on devices. In a competitive marketplace, this strategy has limits.
• Dispense higher technology, premium products. In most practices, pursuing this strategy has the greatest upside. When patients understand the advantages of higher performance products, most are willing to co-pay for the difference between the product’s price and their insurance allowance. Here, effective education on product benefits pays off.
As independent ECPs increasingly rely on managed care payments to stay afloat, it becomes increasingly necessary that they manage their product mix to assure adequate profitability. In broad terms this means offering patients high-technology products with unique benefits that can command premium fees and create high patient satisfaction and loyalty.
In eyewear, it means educating patients about new lenses that improve the personalization of the fit. In contact lenses, it means upgrading patients to the latest technology products and fitting specialty lenses, such as those offered by companies like SynergEyes, that address needs not as well satisfied by mass marketed lenses.
Many ECPs have learned that a dispensing strategy emphasizing high-technology products is successful at overcoming a managed care patient’s natural inclination to avoid out-of-pocket expense. As such, the strategy can offset the profit shrinkage caused by the managed care reimbursement squeeze.
Thomas F. Steiner, Director of Market Research for ROB, has spent more than 25 years helping eyecare practices succeed, including pioneering the introduction of color contact lenses into optometry. To contact him: tnlsteiner@comcast.net





















