By Jerry Godwin, MBA

Article 1in the ROB series:”Getting on Track with the Medical Model.”
SYNOPSIS
Most practices derive less than 20 percent of revenues from medical model optometry—a percentage that can be doubled. The first step toward growth: Measure your starting point.
ACTION POINTS
BENCHMARK. Measure your medical eyecare services by percent of exam and revenue, then compare those figures to national norms.
SET GROWTH GOALS. Aim to double revenues from medical eyecare services; for most practices, it is doable. Then set goals to improveother performance metrics.
PUT A PLAN IN MOTION. Construct and implement a plan to deliver medical eyecare (logistics) and be compensated for the work that you do (billing and coding).
Optometry has expanded its scope of practice to include the delivery of medical eyecare services. Yet, progress falls short of potential: Today, optometric practices, on average, derive less than 20 percent of practice revenues from medically billed eyecare services.
At Optometric Medical Solutions, we have a lot ofexperience in providing comprehensive management services and systems to optometric practices, and we find that doubling the revenue contribution from such servicesis an achievable goal.
We work withpractices that have moved from billing little-to-no medical insurances to generating over $80,000 in the first year. We have also worked with practices that have seen medical billings increase only 10 percent, yet their income rose 15 percent. This is due to the moreefficient and effective billing and collections of patients already being seen in the practice.
To succeed in growing your medical eyecare services, you need to set a goal, construct a plan—then execute that plan. You may need to refocus your practice, making it medically focused. But before any of that, you need to see where you are.
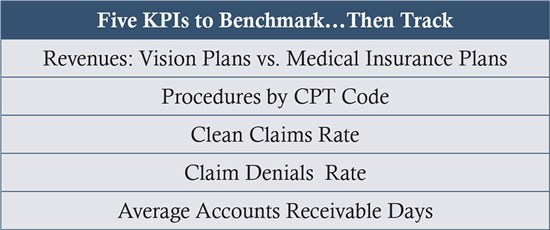
Identify Key Performance Indicators
The benchmarking process begins by identifying Key Performance Indicators (KPIs) and measuring them in your practice. Use the past three- to six-month average as baseline.
Revenues: Vision Plan vs. Medical Insurance
Sort your billings for the past three- to six-monthsby third-party vision plans (e.g.,VSP, Davis, Spectera) vs. third-party medical plans (e.g.,UHC, Blue Cross/Blue Shield). Compare to the national benchmark. Note your starting point and set an improvement goal.
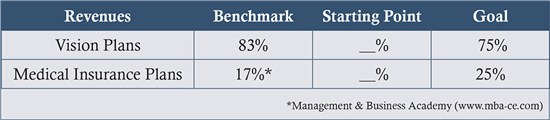
Discussion: Typically, a practice derives 17 percent oftotalrevenuesfrom claims filed to medical insurance. If you are achieving this level, you should set a goal of billing 25 percent to medical insurance. The average practice, among those we consult to, files 135 claims per month or 1,620 per year. These claims generate $22,486 per month or $269,832 per year.
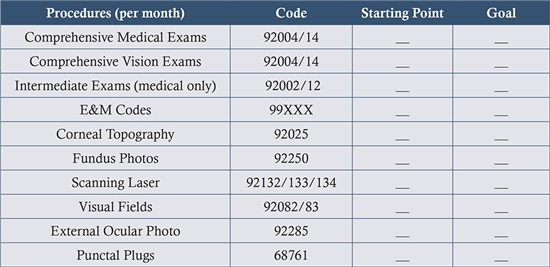
Procedures by CPT Code
List the CPT (procedure) codes that you currently use to provide care for patients billed to medical insurance payers. Set monthly targets for these codes Then review them weekly to assess progress in achieving your targets. Determine if you need to expand your usage of procedures based on the pathology seen (i.e.: diabetic, glaucoma, dry eye, allergy, AMD, etc.) compared to protocols for clinical care. Click HERE to view the AOA Clinical Guidelines.
Clean Claim Rate
Measure your clean claim rate, the rate at which your claims are successfully passing through to payers for processing. A claim is considered clean if a payer or intermediary never rejected it. Calculate it by dividing the number of claims never rejected by the total claims filed over a selected time period.

Claim Denial Rate
Measure the claim denial rate, the percentage of claims denied, trending over a selected time period. Calculate this by dividing the number of Denied Remits by the number of Total Remits returned for all payers during the selected time period. Benchmark target is 2.5 percent.
DISCUSSION: Achieving goals for Claim Rates is a product of setting in place protocols for coding and billing claims. A practice can do this itselfor by contracting with an outside service. The key: establishing a comprehensive system for a revenue cycle.When a practice incurs a denial, something is wrong with its claims filing, patient demographics or insurance verification process. A practice can determine the problemfrom the denial reason code, and then adjudicate the claims based on missing or incorrect data submitted. Importantly, a practice should implement office processes and protocols to avoid this issue occurring again.

Average Accounts Receivable Days
Measure the Accounts Receivable (AR) Days, the number of days from date of service to payment. AR Days calculates the time it is taking to receive payment from the date of service (DOS) until you receive reimbursement.
This can be broken down into two segments: days-to-payer-receipt and days-to-payment. Days-to-payer-receipt represents the time it takes you to submit the claim to the payer and the payer to acknowledge receipt of the claim. In contrast, the days-to-payment represents the time it takes for the payer to process the claim.Add these two periods to computetotal AR Days.
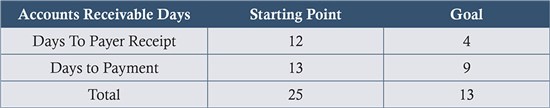
DISCUSSION: Ultimately, a claim should be filed the day that services are rendered. In a practical world, however, a practice needs to build in time for scrubbing the claim (that is, reviewing the claims and correcting any errors), a process often conducted by an intermediary between provider and payer. Thebest-performing practice we’ve worked with averages just four days to payer receipt, then nine more days to payment, for a totalturnaround of 13 days. This level of efficiencyis a product ofmeticulous adherence to the protocols that we lay out for the practice.
Brent Schmidlap, OD, opened Rockwall Precision Eye Care in Rockwall, Texas, in 2007. After six months, he sought the help of a consultant to add and implement the medical model. Working with the consultant, Dr. Schmidlap and his staff of three were credentialed on medical panels, set up administrative processes, including a revenue cycle platform, and began to focus on implementing the key elements of the medical model. In 10 months, the practice went from zero revenue to generating $80,000 in medical eyecare services. Today, medical eyecare represents 21 percent of patient care revenues in his practice.
Jerry Godwin, MBA, is CEO of Optometric Medical Solutions, based in San Antonio, Texas. OMS is a leader in providing comprehensive management services and systems to optometric practices and a “change agent” in helping practices to embracethe medical model.To reach him: jgodwin@optmedsol.com

























